By: Gina M. Poisson, MS, LMFT, MedFT-C
It is a privilege to work as a Medical Family Therapist (MedFT) at the Oklahoma City Indian Clinic. “Medical Family Therapy (MedFT) is a form of professional practice that uses the biopsychosocial model and systemic family therapy principles in the collaborative treatment of individuals and families dealing with medical problems.” (McDaniel, S.H., 2014). Additionally, research has also shown that a family systems approach can also be useful for strengthening family support when individuals are facing serious health issues. (Cherry, 2022)
The Oklahoma City Indian Clinic Integrated Health team has 6 dedicated Medical Family Therapists: Alicia Barber, LPC, LADC is assigned to the Women’s Clinic, Charlie Moore, LPC is assigned to the Metabolic Clinic, Nolan Lawless, LPC is assigned to both the Red and Blue Primary Care teams, Phillip Thomson, LMSW is assigned to the Sage and Gold Primary Care teams, Taylor Bankston, LPC-C is assigned to Pediatrics and I, Gina Poisson, LMFT (Manager of Integrated Health), am assigned to the Easy Access Team.
In addition to issues normally presented in an outpatient therapy setting; as MedFTs we have the opportunity to work with patients to address issues including diabetes, ADHD, sleep apnea, transgendered patients seeking hormone replacement therapy (HRT), chronic pain, chronic illness, substance abuse, patients in crisis, cancer patients, and prenatal and postpartum issues.
Primary Care Partners, a group practice in Grand Junction, Colo., with 21 family physicians and 14 pediatricians reported the following benefits of incorporating Behavioral Health Specialists (aka MedFTs) into their practice:
- “Increased efficiency. Chronically ill patients with co-occurring somatic or mental health issues can be quickly sent to an in-house behavioral health specialist without a referral or scheduling a separate appointment. All the while, the physician is able to remain on schedule.
- Increased patient and physician satisfaction. Both patients and physicians report that they prefer the convenience, efficacy and support of on-site behavioral health specialists.
- Improved health outcomes. Working as a team, the physician and behavioral health specialist assist the patient in managing chronic illnesses that often require changes in lifestyle and behaviors.
- Improved mental health outcomes. Research shows that patients with mental health conditions achieve greater symptom relief and have less need for costly emergent services when treated by an interdisciplinary team.” (Reitz, R, 2011)
Medical Family Therapy continues to be an ever-evolving family systemic profession as more MedFTs’ skills are requested by physicians, medical clinics and hospitals across the nation.
The goal of this article is to share some beneficial practices as a MedFT working with the Native American population. In this article, the terms “Indigenous,” “Native(s),” “Native American” and “American Indian(s)” are used interchangeably. While I have the lens of a Marriage and Family Therapist as well as that of a Medical Family Therapist, any mental health discipline would find these important considerations at the very least noteworthy in working with Indigenous populations.
Begin with a Client Centered approach
“Person-centered therapeutics is the use of an interpersonal alliance and humanistic dialogue to orchestrate lifestyle change and other procedures as needed to heal illness, prevent disease and promote health. Randomized controlled trials of person-centered treatments that promote well-being have lower drop-out, relapse and recurrence rates than other treatment approaches. For therapeutics to be effectively person-centered, it must involve an awareness and respect for the whole person, whose health is certainly more than his or her symptoms of illness and past medical history. The unique experiences, goals, and values of each person are assessed and treated in a person-centered therapeutic alliance, which optimally seeks to promote complete physical, mental, social, cultural and spiritual well-being. Person-centered therapeutics addresses the needs of the person (of the totality of the person’s health, both ill and positive aspects), and are engaged by the person (with clinicians extending themselves as full human beings), for the person (assisting the fulfillment of the person’s health aspirations and life project), and with the person (in a respectful and empowering relationship with the person who consults). Essentially, person-centered therapeutics is a practical application of the science of well-being to health care and health promotion.” (Cloninger, R., 2011)
Think about what Native American history you are aware of, and at some point your mind goes to what Native Americans sacrificed: land, people, culture, language, etc. The client-centered approach bodes well for the Native American population as it requires a non-judgmental and empathetic environment. To better understand the Native American patient requires understanding the Indigenous’ intergenerational trauma and a keen ability to provide a biopsychosocial approach, sometimes just by listening to the stories about the ancestral heritage of the patient. MedFTs are especially challenged in attaining as much information as they can in a span of 15 to 20 minute visits. Like most first encounters, it is establishing rapport and the building of trust that is needed to offer further assessment and treatment.
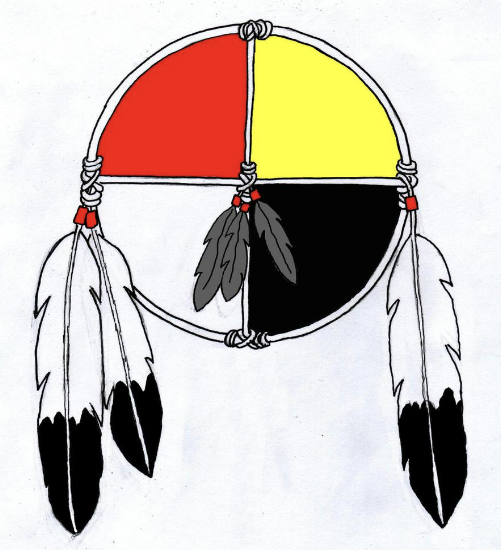
The Medicine Wheel is our guide
When assisting Native American patients, the Medicine Wheel is a symbol that provides an accessible and easily referenced framework to ensure all areas of the patient and their concerns are addressed. The Medicine Wheel holds different meanings to different Indigenous groups; some equate the colors with seasons, some with directions like that of a compass and for some it holds gifts of connectedness through the development process. Using the Wheel as a referenced framework is a reminder of what so many patients seek, and that is to remain balanced.
“Mental wellness is a balance of the mental, physical, spiritual, and emotional. This balance is enriched as individuals have:
- PURPOSE in their daily lives whether it is through education, employment, care-giving activities, or cultural ways of being and doing; indicating physical wellness.
- HOPE for their future and those of their families that is grounded in a sense of identity, unique Indigenous values, and having a belief in spirit; indicating spiritual wellness.
- BELONGING and connectedness within their families, to community, and to culture; indicating emotional wellness.
- MEANING and an understanding of how their lives and those of their families and communities are part of creation and a rich history; indicating mental wellness.” (Restoule, B., 2019)
MedFTs emphasize the importance of offering a biopsychosocial-spiritual (BPSS) approach. Completing a BPSS interview addresses a patient’s physical, mental, emotional and spiritual wellbeing and provides the MedFT the ability to ensure the patient receives a balanced approach. While the interview is lengthy it is not likely to be completed in the first encounter in the exam room. In adhering to the short timeframe, MedFTs are equipped to provide Brief Solution Focused and Motivational Interviewing approaches. The flow and pace of patient engagement is succinct and preventatively focused to provide quality services for improving health outcomes.
Know and appreciate the history of Indigenous people
The history of Indigenous people is a history layered with waves of injustice and disparities. In working with Native Americans it is important to know the history of their ancestors’ plight and the obstacles that were met with sacrifice, perseverance and strength.
MedFTs are aware of the history of the forced acculturation of the American Indians and now implement holding space to honor the enculturation of the Indigenous.
“Enculturation is the connection to tribal culture in terms of identity, participation, and experience. The degree to which an AI person adheres to tribal cultural values and ways has the potential to play an important role in his or her physical health and emotional wellbeing.” (Montgomery, D. et al. n.d.)
When we hold space for another person we are fully present with that person physically, mentally, emotionally and spiritually. Additionally, holding space is a client centered approach that validates whatever the patient brings to the table and requires that the therapist put aside any set agenda to attune to the patients’ immediate needs.
Acknowledge effects of intergenerational trauma
Intergenerational trauma is a history of what families, communities and, in our example, what Native American nations have passed down from one generation to the next.
The effects of intergenerational trauma are evident in what we see in the exam room today. The challenges of this trauma are evident in these facts:
“The rates of substance abuse among Native Americans are generally much higher than those of the general U.S. population. Data indicate that Native Americans have the highest rates of alcohol, marijuana, cocaine, inhalant, and hallucinogen use disorders compared to other ethnic groups.” (Kaliszewski, M. 2022)
- American Indian or Alaska Native (AI/AN) persons, those that are not Hispanic or Latino have the highest rates of suicide than any other racial or ethnic group.
- Suicide rates among non-Hispanic AI/AN persons increased nearly 20% from 2015 to 2020. While the U.S. population reports an overall 1% decrease.
- Knowing what prevention strategies to implement means gaining an understanding of the attributes of the suicide for both American Indians and Alaska Natives.(Stone, B., 2022)
Kyla Molina, (2022) Licensed Professional Counselor, Doctoral Candidate and Oklahoma City Indian Clinic Pediatric clinician, shared the following in her dissertation proposal:
Historical trauma, intergenerational trauma, acculturation and enculturation comprise the foundation of the Native persons’ identity. She hypothesized how Indigenous people think about their past, their present and what hope they have for their future presents a direct link to levels of depression, anxiety levels, and their overall mental and physical well-being.
Molina further shares, based on US bureau of labor statistics, that the following economic disparities have a direct effect on how Native people view their current experiences and ability to improve their four areas (mental, physical, emotional and spiritual) of a balanced life.
- “Lack of resources-is leading to poverty and unemployment.
- In the U.S. 1 in 3 Native Americans are living in poverty; the average individual earning a median income of just 23,000/yr.
- Living conditions for Natives people are dire, examples include living in temporary housing for longer periods of time.
- American Indian and Alaska Native household are more likely to face homelessness or live in significantly overcrowded conditions
- Native American students have lower high school graduation rates than other ethnic groups.
- The high dropout rate can be attributed to poor education systems that do not accommodate many indigenous students’ needs.”
Despite these economic issues, there are major efforts within our community to foster and generate resilience. By creating connections, providing access to resources, increasing knowledge on wellness, and telling our stories.” (Molina, 2022)
Acknowledge the resilience and strength of the Indigenous people
Cultures as rich and diverse as those of the American Indians cannot be summarized in a few words. Native Americans have shared their story with us in many ways through the telling of their history, through the preservation of their languages, through song, all of which communicate strength and perseverance.
MedFTs acknowledge the family members’ influence and are in a unique position to express empathy for family members who have daily influence as well as honoring a patient’s ancestors who have impacted their lives. These acknowledgements are essential in this time of post-COVID. Many tribal elders died while in the beginning stages of sharing traditions, ceremonial structure and language, and thus these have to be rebuilt and embraced by those that remain.
Acknowledge effects of the pandemic and loss
There is no doubt the forced isolation of the pandemic caused an unwanted ripple of increased anxiety and depression across our nation. The C.D.C revealed that Native Americans experienced massive death tolls due to COVID. Additionally, from 2019 to 2021 the Native Americans’ life expectancy fell from 71.8 to 65.2. The main causes of these deaths appear to be connected to poverty, having a higher rate of underlying health problems that exacerbate COVID and having limited access to health care. (Lopez & Wu, 2022)
I, along with Alicia Barber, LPC and Phillip Thomson, LMSW lead a grief group at the clinic. We facilitate these groups both in person and online. As MedFTs, we hear firsthand the gravity of the multiple deaths that resulted for American Indians. Leading these groups provides an educational opportunity for patients to hear the loss of others and bear witness to each other’s grief. These groups are another example of the importance of holding space. The space must be experienced as emotionally safe for group participants to share the effects of their recent losses.
Be mindful without stereotyping
MedFTs are mindful of the Native culture influences and how the patient constructs their belief as to why their illness exists as well as how the patient views their potential to heal. It is essential to stay clear of stereotyping and consider the following generalizations which may be true for some Native Americans but not for all:
Communication
- Anecdotes or metaphors may be used.
- Long pauses generally indicate that careful consideration is being given to a question. Do not rush patient.
- Direct eye contact may be avoided out of respect and/or concern for soul loss/theft.
- Loudness is often associated with aggressiveness among Navahos and should be avoided
- Due to the history of misuse of signed documents some may unwilling to sign informed consent or advance directives.
- Older Adults may prefer the term “American Indians” over “Native Americans.”
Expression of Pain
- Stoicism is often highly valued and patients may not express their pain other than by mentioning, “I don’t feel so good.” or “Something doesn’t feel right.”
Health Related Practices
- Before cutting or shaving hair, check to see if patient or family wants to keep it. Realize that in some tribes cutting hair is associated with mourning.
- A medicine bag may be worn. Do not treat it casually or remove it without discussing it with the patient. Allow a family member to remove it, if it must be removed. Keep it close to the patient as possible and return it as soon as possible.
- Food that is blessed may be thought to be devoid of harm.
- Traditional healers may be combined with use of Western medicine.” (Galanti, 2008)
Through each of the aforementioned essential considerations, rest assured that the OKC Indian Clinic MedFTs embrace a collaborative approach in working with both the patient and the medical providers. While every day is different and there are many unknowns, we remain inquisitive to learn and apply the best practices to address the needs of the Native American patient. We consider it an honor to provide health services to American Indians and in meeting patients where they are at in their journey to the balanced life they seek.
References
Cherry, K. (2022, November 14). What is Client-Centered Therapy? Verywell mind. https://www.verwellmind.com/client-centered-therapy-2795999
Cloninger, C.R. et al. (2011, April). Person Centered-Therapeutics. The National Library of Medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4454449/
Galani, G. Caring for Patients from Different Cultures. University of Pennsylvania Press, Philadelphia, Pennsylvania. 2008, p. 239-241.
Kaliszewski, M. (2022, September 12) Alcohol and Drug Abuse among Native Americans. American Addiction Centers. https://americanaddictioncenters.org/rehab-guide/addiction-statistics/native-americans
Lopez & Wu. (2022, September 8). Covid’s Toll on Native Americans. The New York Times, The Morning Newsletter. https://www.nytimes.com/2022/09/08/briefing/covid-death-toll-native-americans.html
McDaniel, Susan H., et al. Medical Family Therapy and Integrated Care, second ed., American Psychological Association, Washington, DC, 2014, p. 9
Molina, K (2022, November). Evidence based treatment for youth and families with an emphasis on indigenous people [Dissertation Presentation].
Montgomery, D. et al. (n.d.) “Development of the American Indian Enculturation Scale to Assist Counseling Practice.” Research Paper. 15(2) Front End.indd (ed.gov)
Reitz, R. et al. (2011, Jan/Feb ed.) FPM Journal. Fam Pract Man. Integrating a Behavioral Health Specialist into your practice. Fam Pract Manag. 2011;18I1):18-21. www.aafp.org/pubs/fpm/issues/2011/0100/p18.html
Restoule, B. (2019, May 23). Returning to the teachings of health and wellness [Conference presentation]. Primary Care & Wellness Summit, FNHA Keynote. https://www.fnha.ca/Documents/FNHA-PCMHW-Summit-2019-Presentation-Dr-Brenda-M-Restoule.pdf
Stone, D. et al. (2022, September 16). Suicides Among American Indian or Alaska Native Persons — National Violent Death Reporting System, United States, 2015–2020. Center for Disease Control. Suicides Among American Indian or Alaska Native Persons — National Violent Death Reporting System, United States, 2015–2020 | MMWR (cdc.gov)
Bio: Gina Poisson, LMFT is a licensed marriage and family therapist and an AAMFT Clinical Fellow. Her educational background includes a BS in Family Relations and Child Development from Oklahoma State University, Stillwater, OK, a MS in Family Therapy from Friends University, Wichita, KS, and Certification in Medical Family Therapy from Oklahoma Baptist University, Shawnee, OK. Poisson is currently the manager of Integrated Health/Medical Family Therapy at Oklahoma City Indian Clinic. Poisson leads a team of five Medical Family Therapists and two Peer Recovery Specialists. Together Poisson and the Integrated Health team meet with Native American patients during their medical appointments; the goal is to assist patients in attaining better health outcomes.
Special thanks and recognition to:
Kyla Molina, LPC, Doctoral Candidate for her contribution to this article.